Introduction
Typhoid fever is a bacterial infection caused by Salmonella enterica serotype Typhi (S. Typhi) bacteria. It is a significant global health concern, particularly in areas with poor sanitation and limited access to clean water. In this blog post, we will explore the causes, symptoms, diagnosis, treatment, medication, dosage, and prevention strategies for typhoid fever. By understanding this disease and its management, we can take necessary precautions and promote better public health practices.
Causes of Typhoid Fever
Typhoid fever is primarily caused by consuming food or water contaminated with the feces of an infected person. This can occur due to inadequate sanitation, improper food handling, or the use of contaminated water sources. The S. Typhi bacteria then enters the digestive system and spreads throughout the body, causing the characteristic symptoms of typhoid fever.
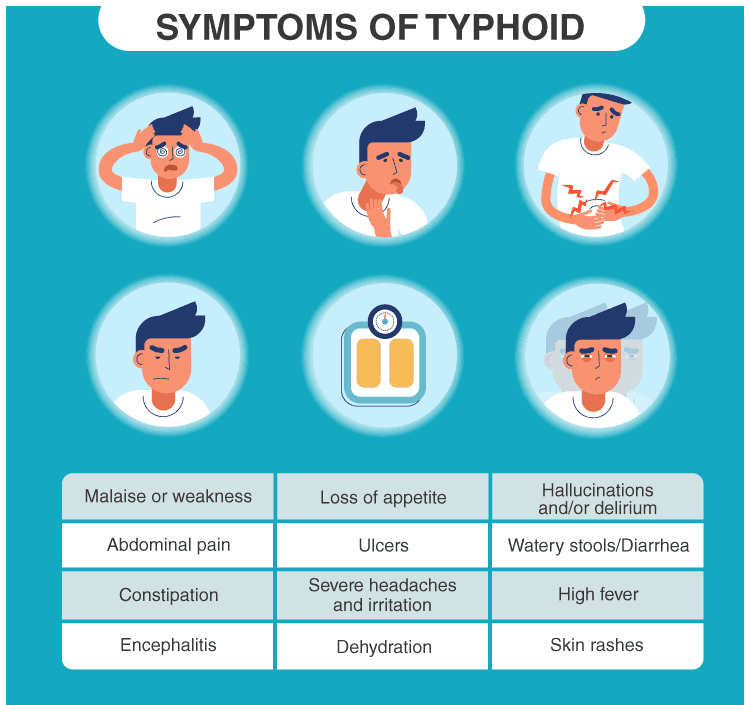
Symptoms of Typhoid Fever
The symptoms of typhoid fever usually develop within 1 to 3 weeks after exposure to the bacteria. Common symptoms include high fever, headache, abdominal pain, loss of appetite, and generalized weakness. Patients may also experience a rose-colored rash, constipation, or diarrhea. If left untreated, severe complications such as intestinal perforation or infection in other organs can occur.
Diagnosis of Typhoid Fever
Diagnosing typhoid fever involves various methods, including:
Blood Culture: This is the most reliable method for identifying the presence of S. Typhi bacteria. Blood samples are collected and cultured to isolate the bacteria for further analysis.
Stool Culture: In some cases, stool samples may be collected to detect the bacteria. However, this method is less sensitive than blood culture.
Serologic Tests: These tests detect antibodies produced by the body in response to the S. Typhi bacteria. They can be helpful in confirming a recent or past infection.
Treatment of Typhoid Fever
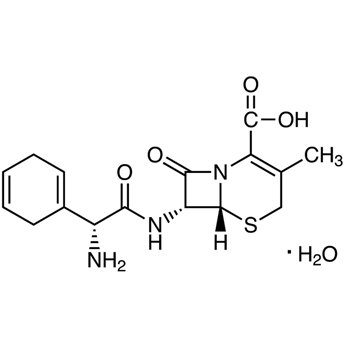
Prompt treatment is crucial to manage typhoid fever and prevent complications. The mainstay of treatment involves the use of antibiotics to eliminate the bacteria. Commonly prescribed antibiotics include fluoroquinolones (e.g., ciprofloxacin), cephalosporins (e.g., ceftriaxone), and azithromycin. The choice of antibiotic depends on factors such as the patient’s age, drug resistance patterns, and the severity of the infection.
It is important to complete the full course of antibiotics as prescribed by a healthcare professional to ensure eradication of the bacteria. In severe cases or when complications arise, hospitalization may be required for intravenous administration of antibiotics and supportive care.
Medication and Dosage
The dosage and duration of medication for typhoid fever depend on several factors, including the patient’s age, weight, and the severity of the infection. It is essential to follow the prescribed dosage and complete the entire course of antibiotics to ensure effective treatment.
Ciprofloxacin: The typical dosage for adults is 500 mg orally twice daily for 10-14 days. For children, the dosage is based on body weight and determined by the healthcare provider.
Ceftriaxone: The usual dosage for adults and children is 1-2 grams once daily intravenously or intramuscularly for 10-14 days.
Azithromycin: The recommended dosage for adults is 500 mg orally once daily for 7-10 days. Pediatric dosage is determined by the healthcare provider based on the child’s weight.
It is crucial to consult with a healthcare professional for accurate dosing instructions and any specific considerations.
Prevention of Typhoid Fever
Preventing typhoid fever involves implementing several key measures, including:
Vaccination: Vaccines such as the Vi capsular polysaccharide vaccine and the Ty21a live oral vaccine can provide protection against typhoid fever. Consult with a healthcare professional to determine the appropriate vaccination schedule and suitability for your specific circumstances.
Safe Food and Water Practices: It is crucial to consume safe and hygienically prepared food. Drink clean, treated water and avoid ice or beverages prepared with untreated water. Proper hand hygiene, including regular handwashing with soap and clean water, is essential.
Sanitation and Hygiene: Improve sanitation facilities and promote proper waste management to reduce the risk of contamination. Educate individuals and communities on the importance of personal hygiene practices.
Travel Precautions: When traveling to areas with a high risk of typhoid fever, take necessary precautions such as consuming only cooked foods, drinking bottled or boiled water, and avoiding street food or raw fruits and vegetables.
Health Education and Awareness: Promote awareness campaigns to educate communities about the causes, symptoms, and prevention of typhoid fever. Encourage early medical consultation for suspected cases.
Conclusion
Typhoid fever remains a significant public health concern, particularly in areas with poor sanitation and limited access to clean water. By understanding the causes, symptoms, diagnosis, treatment, medication, dosage, and prevention strategies for typhoid fever, we can take proactive steps to protect ourselves and others from this bacterial infection. Vaccination, safe food and water practices, improved sanitation, and health education are vital components of comprehensive prevention efforts. Remember to consult with healthcare professionals for accurate diagnosis, appropriate treatment, and specific guidance on medications and dosages. With increased awareness and collective action, we can work towards reducing the burden of typhoid fever and improving global health outcomes.